The discovery of colon polyps during a routine screening creates an immediate mix of relief and concern – relief that early detection occurred, yet worry about how this finding could affect your ability to secure life insurance. Many individuals assume that any abnormal findings automatically complicate the process, while others wonder if they should delay applying until after polyp removal.
The reality is that most colon polyps, particularly benign ones, have minimal impact on life insurance eligibility when properly documented and managed. Insurance underwriters understand that polyps are incredibly common – affecting up to 40% of adults over 50 – and have developed nuanced approaches to evaluate applications based on polyp type, size, and removal success.
Our analysis of hundreds of cases reveals the coverage strategies that work best for individuals with colon polyps, from immediate approvals for routine findings to specialized approaches for more complex situations.
“Most people with routine colon polyps can obtain standard or near-standard life insurance rates, especially when polyps are completely removed and pathology shows benign findings. The key is timing your application correctly and working with carriers that understand colorectal health.”
– Insurance Brokers USA Team
About the Author
The Insurance Brokers USA Team consists of licensed insurance professionals with extensive experience helping clients with complex health conditions find appropriate coverage. Our agents have worked with hundreds of individuals facing colorectal health concerns, specializing in alternative insurance solutions when traditional coverage requires additional consideration.
Table of Contents
- How Do Insurance Companies View Colon Polyps?
- When Should You Apply for Coverage?
- What Factors Affect Your Application?
- What Coverage Options Are Available?
- What Medical Records Do You Need?
- How Will This Affect Your Premiums?
- What Are the Best Application Strategies?
- Frequently Asked Questions
How Do Insurance Companies View Colon Polyps?
Key insight: Insurance underwriters approach colon polyps with a risk-stratified methodology that considers the significant difference between benign polyps and those with malignant potential. Most carriers understand that polyp detection and removal demonstrate proactive health management rather than indicating an increased mortality risk.
The underwriting process typically categorizes colon polyps into distinct risk levels. Hyperplastic polyps, which account for approximately 90% of all polyps found during screening, are considered to have virtually no additional risk by most insurers. These small, benign growths rarely progress to cancer and often result in standard rate approvals when properly documented.
Bottom Line
Routine benign polyps discovered during screening colonoscopy typically have minimal to no impact on life insurance rates, especially when completely removed with clear pathology reports.
Adenomatous polyps receive more careful evaluation, as these represent the type most likely to develop into colorectal cancer over time. However, even adenomatous polyps that are completely removed with negative margins rarely result in coverage denials. Instead, insurers focus on factors such as polyp size, number, degree of dysplasia, and the completeness of removal.
Fortunately, the insurance industry’s approach reflects the current medical understanding that successful polyp removal significantly reduces the risk of colorectal cancer below that of the general population. This preventive benefit often works in favor of applicants who maintain regular screening schedules and demonstrate consistent follow-up care.
Key Takeaways
- 90% of polyps are hyperplastic and considered to have no additional risk
- Complete removal with clear margins typically results in standard rates
- Regular screening demonstrates proactive health management
- Adenomatous polyps require more documentation, but rarely cause denial
When Should You Apply for Coverage?
Key insight: Optimal application timing depends primarily on having complete pathology results and demonstrating successful polyp removal rather than waiting for arbitrary time periods. Most carriers prefer applications submitted 30-90 days after polyp removal when all medical documentation is available.
The traditional approach often involves waiting six months to one year after polyp discovery, but this strategy can unnecessarily delay important financial protection. Our recommended strategy involves applying once you have comprehensive documentation, including colonoscopy reports, pathology results, and evidence of complete removal.
Timing Strategy by Polyp Type
| Polyp Type | Optimal Application Timing | Required Documentation |
|---|---|---|
| Hyperplastic (small) | 30-60 days post-removal | Colonoscopy report, pathology |
| Adenomatous (low-grade) | 60-90 days post-removal | Complete pathology, follow-up plan |
| Large or multiple polyps | 90-120 days post-removal | Comprehensive records, surveillance schedule |
For individuals discovered to have polyps during routine screening, immediate application may be possible if the polyps are small, completely removed during the same procedure, and pathology confirms benign findings. This approach works particularly well for hyperplastic polyps under 5mm that show no concerning features.
“Don’t let perfect timing prevent good timing. If you need life insurance now and have benign polyp findings with complete removal, apply with proper documentation rather than waiting for an arbitrary timeframe that may not improve your rates.”
– Senior IBUSA Underwriter
The exception to immediate application occurs when polyps show high-grade dysplasia or when removal is incomplete. These situations benefit from waiting until a repeat colonoscopy confirms successful management and no residual abnormal tissue remains.
Bottom Line
Apply 30-90 days after polyp removal once you have complete documentation, rather than waiting for arbitrary time periods that don’t improve your underwriting outcome.
What Factors Affect Your Application?
Key insight: Insurance underwriters evaluate colon polyps using a comprehensive risk assessment that weighs multiple factors simultaneously, with polyp histology and removal completeness carrying the most significant weight in determining final rates.
The primary underwriting factors include polyp type and histology, with hyperplastic polyps receiving minimal attention compared to adenomatous polyps that require detailed evaluation. Size becomes increasingly important for polyps over 10mm, as larger adenomatous polyps carry higher malignant potential and may trigger additional rating factors.
The number of polyps influences underwriting decisions, particularly when multiple adenomatous polyps are present. However, the presence of numerous small hyperplastic polyps typically doesn’t impact rates significantly, as these represent common age-related findings rather than meaningful cancer risk factors.
Key Takeaways
- Polyp histology (type) is the most important factor
- Complete removal with clear margins prevents rating increases
- Size matters most for adenomatous polyps over 10mm
- Multiple small hyperplastic polyps rarely affect rates
- Family history of colorectal cancer adds complexity
Removal technique and completeness significantly impact underwriting outcomes. Polyps removed in their entirety with clear pathologic margins receive standard evaluation, while those requiring piecemeal removal or showing incomplete excision may trigger postponement until follow-up confirms successful management.
Age at discovery plays a crucial role in risk assessment. Polyps discovered during age-appropriate screening (typically after age 45-50) receive different consideration than those found in younger individuals, where early onset may suggest hereditary factors or higher baseline risk.
Family history of colorectal cancer, particularly in first-degree relatives, compounds the underwriting evaluation. However, most carriers recognize that early detection and removal in individuals with a family history actually reduces their risk compared to those with similar family history who don’t undergo screening.
Bottom Line
Complete removal of benign polyps with clear pathology typically results in standard rates, regardless of size or number, when discovered during routine screening.
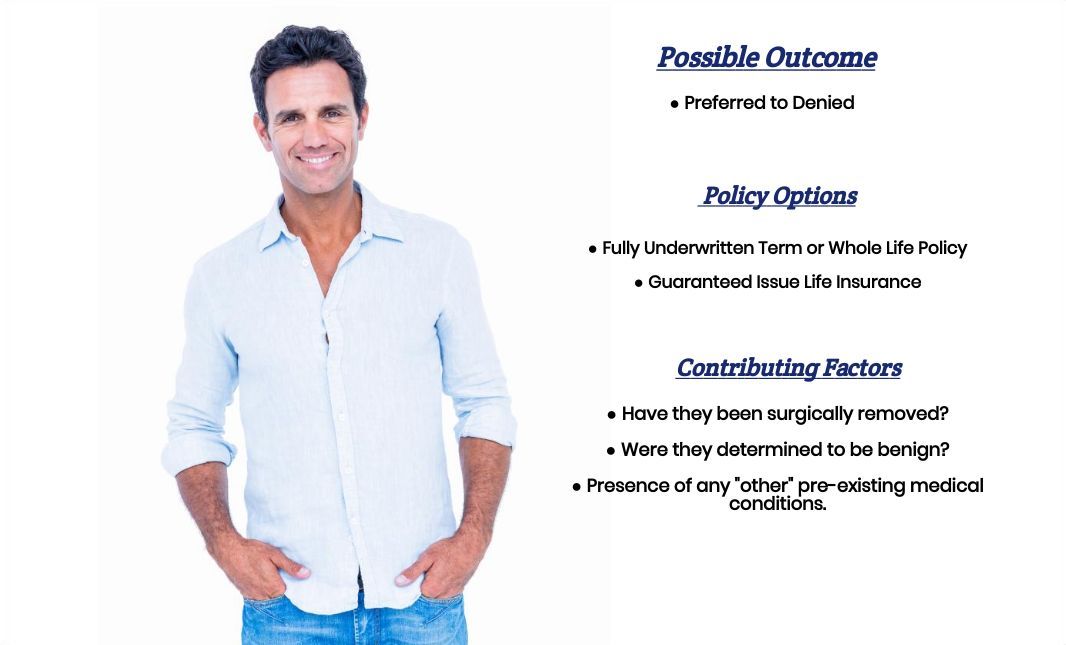
What Coverage Options Are Available?
Key insight: Individuals with colon polyps typically qualify for the full spectrum of life insurance products, from traditional term and whole life policies to no-exam life insurance options, with product selection depending more on coverage needs than polyp history.
Traditional underwritten policies remain the primary option for most applicants with a polyp history. These policies offer the best rates and highest coverage amounts, particularly when polyps are benign and completely removed. The medical exam and underwriting process allow carriers to properly evaluate the low risk associated with successfully managed polyps.
No medical exam policies provide an alternative path for individuals who prefer to avoid detailed medical questioning or those with more complex polyp situations. While these policies typically carry higher premiums, they can be valuable for people with adenomatous polyps, incomplete removal, or surveillance concerns who might face rating increases with traditional underwriting.
Coverage Options by Polyp Situation
| Polyp Situation | Best Options | Expected Outcome |
|---|---|---|
| Hyperplastic, removed | Traditional term/whole life | Standard rates |
| Small adenomatous, removed | Traditional underwriting | Standard to Table 2 |
| Multiple or large polyps | Traditional + no-exam backup | Varies by carrier |
| Recent discovery | No-exam policies | Higher premiums, immediate coverage |
Group life insurance through employers provides another valuable option, particularly for individuals with more complex polyp situations. These policies typically don’t require medical underwriting for basic coverage amounts and can supplement individual policies effectively.
Simplified issue policies offer middle-ground coverage for people who want more than group insurance provides but prefer to avoid extensive medical questions. These products typically ask broad health questions that may not specifically address polyp history, making them suitable for individuals with routine findings.
“The goal isn’t just getting approved – it’s getting the right coverage at fair rates. Sometimes that means traditional underwriting, sometimes it means no-exam policies, and often it means using multiple products to create comprehensive protection.”
– IBUSA Planning Specialist
For individuals seeking substantial coverage amounts, working with top-rated life insurance companies that specialize in medical underwriting provides the best path to competitive rates. These carriers have sophisticated risk assessment capabilities and often provide better outcomes for polyp situations than smaller insurers with limited underwriting expertise.
Bottom Line
All major insurance product types remain available to individuals with colon polyps, with traditional underwritten policies typically offering the best rates for routine polyp situations.
What Medical Records Do You Need?
Key insight: Complete and organized medical documentation significantly accelerates the underwriting process and improves approval odds, with colonoscopy reports and pathology results serving as the cornerstone of your application file.
The colonoscopy report provides essential procedural details that underwriters need to assess risk accurately. This report should include the indication for the procedure, quality of bowel preparation, completeness of examination, detailed description of polyp locations and characteristics, and removal techniques used.
Pathology reports deliver the definitive information that determines underwriting outcomes. These reports must specify polyp histology, degree of dysplasia if present, margins of excision, and any special characteristics that might influence cancer risk assessment.
Key Takeaways
- Colonoscopy procedural reports with complete findings
- Pathology reports with histologic classification
- Follow-up surveillance recommendations
- Previous colonoscopy records if available
- Physician summary letters for complex cases
Documentation of surveillance plans demonstrates ongoing medical management and helps underwriters understand long-term risk management strategies. Records should include recommendations for future screening intervals and any modifications to standard surveillance protocols based on the findings of polyps.
Previous colonoscopy records, when available, provide valuable context about polyp development patterns and baseline colon health. This historical information can be particularly helpful for individuals who have undergone multiple procedures or those with changing polyp characteristics over time.
Documentation Checklist
- Complete colonoscopy procedural report
- Pathology report with histologic findings
- Physician notes from pre- and post-procedure visits
- Surveillance schedule recommendations
- Any follow-up imaging or procedures
- Previous colonoscopy records (if applicable)
For complex cases involving large polyps, incomplete removal, or unusual histologic findings, a physician’s summary letter can provide crucial context that raw medical records might not convey clearly. This letter should explain the clinical significance of findings, treatment approach, and prognosis in language that non-medical underwriters can understand.
Organizing records chronologically with clear labeling significantly improves processing efficiency. Many applications experience delays simply because underwriters must spend excessive time interpreting disorganized medical records rather than evaluating the actual medical situation.
Bottom Line
Complete colonoscopy and pathology reports are essential, but organized presentation and physician context letters can transform complex cases into straightforward approvals.
How Will This Affect Your Premiums?
Key insight: Premium impact varies dramatically based on polyp characteristics, with hyperplastic polyps typically causing no rate increase while adenomatous polyps may result in modest ratings that still provide substantial value compared to policy postponement or denial.
Standard rate approvals are common for hyperplastic polyps of any size when completely removed with benign pathology. These polyps are so prevalent in the general population that most carriers consider them a normal finding rather than a risk factor requiring premium adjustment.
Small adenomatous polyps (under 10mm) with low-grade dysplasia and complete removal typically result in ratings between standard and Table 2, representing premium increases of 0-50% over standard rates. While this represents additional cost, it’s often substantially less expensive than waiting for time to pass or pursuing higher-cost no-exam products.
Premium Impact by Polyp Type
| Polyp Characteristics | Typical Rating | Premium Impact |
|---|---|---|
| Hyperplastic, any size | Standard/preferred | No increase |
| Adenomatous, <5mm | Standard to Table 1 | 0-25% increase |
| Adenomatous, 5-10mm | Table 1 to Table 2 | 25-50% increase |
| Large or multiple adenomatous | Table 2 to Table 4 | 50-100% increase |
Large adenomatous polyps (over 10mm) or multiple adenomatous polyps typically trigger higher ratings, potentially reaching Table 3 or Table 4 levels. However, even these ratings often provide better value than alternative products, and the rates become more competitive as applicants age and standard rates naturally increase.
The presence of high-grade dysplasia significantly impacts rating decisions, often resulting in ratings of Table 4 or higher, though coverage remains available from most carriers. These situations benefit from working with specialized underwriters who understand the difference between high-grade dysplasia that’s completely removed versus invasive cancer.
“Don’t let the perfect premium be the enemy of good coverage. A Table 2 rating on a traditional policy often costs less than standard rates on a no-exam product, and you get better coverage terms and higher limits.”
– Senior IBUSA Underwriting Manager
Age significantly influences the practical impact of ratings. A 25% premium increase that seems substantial at age 30 becomes much less significant at age 50 when base premiums are higher and the absolute dollar difference may favor the rated traditional policy over alternatives.
Carrier selection plays a crucial role in managing premium impact. Some insurers specialize in medical impairments and offer more competitive rates for polyp situations, while others may be overly conservative. Working with experienced agents familiar with carrier-specific underwriting guidelines can save substantial money over the life of the policy.
Bottom Line
Most polyp situations result in standard to modest rating increases, making traditional coverage more cost-effective than alternative products over the long term.
What Are the Best Application Strategies?
Key insight: Successful applications require matching your specific polyp situation with carriers that have favorable underwriting guidelines for your circumstances, combined with thorough preparation and realistic expectation setting.
The multiple carrier approach provides the best outcomes for most polyp situations. Rather than applying to one carrier and hoping for the best, submitting applications to 2-3 carefully selected insurers allows you to compare offers and choose the most favorable terms. This strategy works particularly well for adenomatous polyps, where underwriting outcomes can vary significantly between carriers.
Preparation strategy involves organizing all medical records, obtaining physician summary letters when beneficial, and preparing clear explanations of your polyp situation. Many applications receive suboptimal ratings simply because underwriters lack clear information about polyp characteristics, removal completeness, or current health status.
Key Takeaways
- Apply to multiple carriers for comparison shopping
- Match your situation with carrier-specific strengths
- Organize documentation before starting applications
- Consider backup strategies for complex situations
- Work with agents experienced in medical underwriting
Carrier matching involves understanding which insurers have the most favorable guidelines for your specific situation. Some carriers excel with routine adenomatous polyps, while others provide better outcomes for multiple polyps or surveillance cases. This knowledge can mean the difference between standard rates and significant premium increases.
The backup strategy approach ensures you have coverage options if primary applications don’t yield favorable results. This might involve having no-exam applications ready to submit, maintaining group coverage during the underwriting process, or considering specialized programs for pre-existing conditions.
“The key to successful polyp underwriting is presenting your case as a solved problem rather than an ongoing concern. Show complete removal, benign pathology, and appropriate follow-up – that’s the story underwriters want to see.”
– IBUSA Medical Underwriting Specialist
Timing coordination becomes important when applying to multiple carriers simultaneously. Scheduling medical exams close together prevents changes in health status from affecting comparisons, and completing all applications within a similar timeframe ensures fair rate comparisons.
For complex situations involving large polyps, multiple adenomatous polyps, or unusual histologic findings, consider starting with the most conservative carrier first. This approach allows you to understand the worst-case scenario before submitting to more favorable insurers, and provides valuable insight into how underwriters view your specific situation.
Communication strategy involves being completely honest about your polyp history while presenting information in the most favorable light possible. This means emphasizing complete removal, benign pathology, and appropriate follow-up rather than focusing on the discovery of abnormal findings.
Bottom Line
Strategic carrier selection, thorough preparation, and multiple applications typically yield better outcomes than single-carrier approaches for polyp situations.
Frequently Asked Questions
Can I get life insurance if I have colon polyps?
Yes, most people with colon polyps can obtain life insurance coverage. Hyperplastic polyps typically don’t affect eligibility or rates, while adenomatous polyps may result in standard to moderately increased premiums depending on size, number, and pathology findings. Complete removal with benign pathology provides the best outcomes across all polyp types.
Should I wait to apply until after my next colonoscopy?
Generally, no, if your polyps were completely removed with benign pathology. Waiting for future surveillance colonoscopies rarely improves your underwriting outcome and delays important financial protection. Apply once you have completed documentation of successful polyp removal, typically 30-90 days after the procedure.
Will hyperplastic polyps affect my life insurance rates?
Hyperplastic polyps typically have no impact on life insurance rates. These benign growths are extremely common and considered normal age-related findings by most insurance carriers. Complete removal with pathology confirmation of hyperplastic tissue usually results in standard rate approvals.
What if my adenomatous polyps had high-grade dysplasia?
High-grade dysplasia increases underwriting complexity but doesn’t prevent coverage. These cases typically result in higher premium ratings (Table 3-4 or more) but remain insurable when completely removed with clear margins. Working with specialized underwriters familiar with colorectal pathology provides the best outcomes.
Do I need to disclose polyps found during routine screening?
Yes, you must disclose all polyp findings during the application process. Insurance applications require disclosure of all medical conditions, procedures, and findings. However, polyps discovered during routine screening often demonstrate proactive health management, which can work in your favor during underwriting.
Can I get coverage if my polyp removal was incomplete?
Incomplete polyp removal typically requires postponement until follow-up confirms successful management. Most carriers prefer to see evidence of complete removal or successful repeat intervention before making final underwriting decisions. This usually delays coverage by 3-6 months rather than preventing it entirely.
Should I consider no-exam life insurance instead?
No-exam policies can provide immediate coverage but typically cost more than traditional underwriting for routine polyp situations. Consider no-exam options if you have complex polyp findings, need immediate coverage, or want to avoid detailed medical questions. However, traditional underwriting often provides better rates for straightforward cases.
How does a family history of colon cancer affect my application?
Family history adds complexity but doesn’t prevent coverage, especially with appropriate screening. Carriers recognize that early detection and polyp removal in individuals with a family history actually reduces their cancer risk compared to those with similar family history who don’t undergo screening. Expect additional questions and possibly modest rating increases.